To better understand the information contained in this blog, please read the first three blogs in this series on the endothelial glycocalyx and Nitric Oxide (NO); THE ENDOTHELIAL GLYCOCALYX-PART I, THE ENDOTHELIAL GLYCOCALYX-PART II, and THE ENDOTHELIUM- PART III. This will provide a great education regarding NO and the vascular endothelium, as to how it relates to GI health.
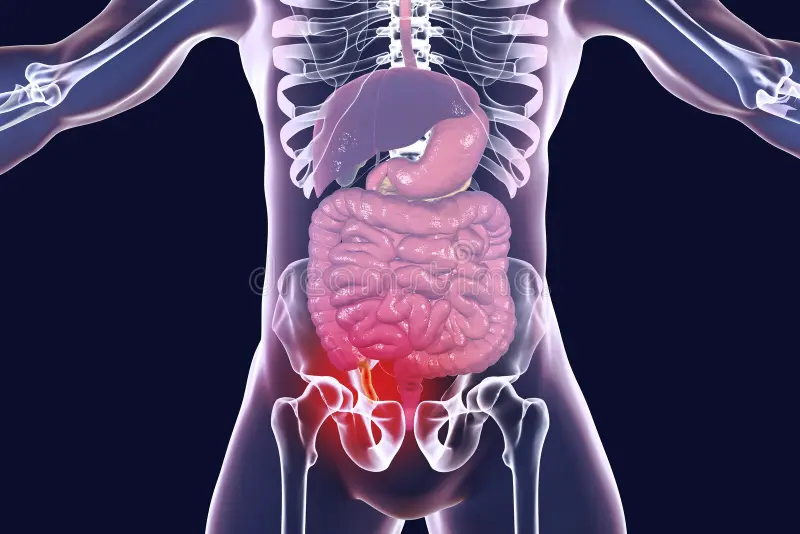
Gastrointestinal (GI) health requires a complex balance of micro-organisms, digestive enzymes, neurotransmitters, hormones, immune system balance, gut-brain, and autonomic nervous system balance. (The importance of the vagus nerve will be the topic of a future blog). Physical and mental well-being requires optimal GI function. The human body contains about 10 trillion cells, the GI tract contains about 100 trillion microbes, or 10x the number of human cells. These microbes contain roughly 2 million genes, the human genome about 20 thousand (100 times fewer genes), so the microbiome has a profound effect on regulating human physical and mental well-being. The root cause of virtually all chronic degenerative conditions may be traced to the GI tract. This makes perfect sense, since there is no other place in the body where the external environment is in such close contact with the internal one (the inside or lumen of the GI tract may actually be considered outside the body, since it is a continuous tube through the body from mouth to anus). The lining of the GI tract (endothelium, enterocytes, or colonocytes) is only one cell thick. Under normal conditions, connections between these cells (tight junctions) regulate the flow of essential nutrients through the cells, while preventing the transport of toxins from the GI lumen into the body. In addition, the body must be able to distinguish self from non-self to prevent the immune system from attacking the body (autoimmune disease) while simultaneously preventing foreign invaders from attacking. This requires a delicate balance between normal and excess immune function. Recognizing self mandates the need for development and maintenance of immune tolerance, a critical role of the GI tract. In fact the majority (about 70%) of the total amount of antibodies are produced in the GI tract.
Among the most rapidly reproducing cells in the body are the colonocytes. Maintenance of normal GI function requires that these cells reproduce/renew themselves about every 6 days. A large amount of energy is needed to do so, as well as are optimal levels of essential nutrients. Failure to keep ideal GI lining leads to GI permeability (a.k.a. Leaky Gut Syndrome), failure of normal GI barrier function, and a cascade of events that are at the root of a host of inflammatory conditions leading to a number of chronic conditions. The remainder of this discussion addresses the importance of nitric oxide (NO) in preserving optimal GI integrity.
Lying between the colonocytes and lumen of the GI tract is a bi-layered mucus membrane, secreted by specialized cells called goblet cells. NO is a signaling molecule that increases mucus secretion and local blood flow (vasodilation), which increases removal of toxins that enter through the GI lining. NO acts by additional means to also: reduce neutrophil adhesion and secretion, reduce oxidative stress from the superoxide free radical, accelerate healing, increase new blood vessel growth, decrease inflammatory cytokines, and reduce histamine release from mast cells, further decreasing inflammation.
As stated above, maintaining the GI barrier is a critical role performed by the colonocytes. Loss of tight junction integrity compromises the GI barrier, and leads to GI permeability. It is known that brain-derived neurotrophic factor (BDNF), a growth factor secreted by a number of different nerve cells to promote nerve survival, growth, and differentiation, also plays a part in intestinal tight-junctions by increasing production of tight junction proteins. NO has a crucial part in the production of BDNF, hence of tight junction upkeep.
The oral and GI microbiomes are closely interrelated, with a significant overlap between the two microbiomes. The intestines are “fed” oral bacteria which then can flourish in the colon. If there is poor oral health (gingivitis, periodontitis, cavities, infected root canals, failure to floss and brush, etc.), the dysbiotic oral bacteria may translocate to the colon, initiating dysbiosis there. As discussed in my last blog, THE ENDOTHELIUM- PART III, there are two independent pathways for the production of NO, an enzymatic pathway involving the conversion of the amino acid arginine to NO, and a second, non-enzymatic pathway called the enterosalivary-Nitrate (NO3) > Nitrite (NO2) > Nitric oxide (NO) pathway. This pathway converts nitrate by certain species of oral bacteria to NO, and requires stomach acid. Dietary nitrites increase nitrite reducing bacteria on the tongue, which acts to decrease dysbiotic oral bacteria, and thus indirectly, dysbiotic colonic bacteria. In this way NO may act as a “natural” antibiotic to reduce dysbiosis.
In a landmark mouse-model study, colitis (Irritable Bowel Disease- IBD) was induced in mice, which were then treated with nitrate (thereby stimulating NO production). Colitis was created by the addition of a 3% solution of dextran sodium sulfate for 5 days in their drinking water. Before that, one group was pre-treated with sodium nitrate (2mM solution) in drinking water for 5 days. The treated group showed significant reductions in inflammation, swelling, bloody stools, maintenance of normal colon length and body weight, decreased elevated white blood cell and lymphocytes. Additionally, immune imbalances typically found in autoimmune IBD’s such as ulcerative colitis, consisting of elevated TH1 and TH17 cells, and decreased Th3 cells, was improved. Similarly, programmed cell death (apoptosis) caused by the induced colitis was inhibited. The anti-inflammatory endothelial nitric oxide (eNOS) pathway of NO production was preserved. Beneficial bacteria species and levels were also maintained in the mice given nitrate. Elevation of a number of signaling pathways associated with cancers, other adverse infectious and biochemical pathways that were stimulated by colitis induction, were prevented by nitrate.
NO has additional immune benefits, including reduction of myeloperoxidase , which when chronically elevated, causes free-radical production and oxidative damage. NO helps regulate mast cell activity and release of histamine. Histamine is the well-known cause of “hay fever”, with itchy eyes, runny nose, and sneezing. In the GI tract, histamine excess alters GI motility, increases permeability, decreases mucosal layer, and acts to inhibit production of NO through the arginine pathway.
In summary, supplementation and dietary nitrates may act via a number of mechanisms to reduce oral and GI dysbiosis, reduce inflammation, improve immune balance, decrease cell death caused by inflammation, decrease histamine release, and improve IBD symptoms. References upon request.
About the Author: Dr. Douglas L. Weed.
Dr. Weed practices Functional Nutrition, Chiropractic care, and offers weight loss solutions in Napa, CA at Heun Chiropractic, Inc. He has a doctorate in Chiropractic care and he has received certifications in physical rehabilitation and as a Qualified Medical Examiner. With a post-graduate certification in Functional Medicine, focusing on functional endocrinology, digestive disorders and Peripheral Neuropathy, he is committed to lifelong education and helping patience transform their health.